When nursing homes get fined for violations, such as nursing home abuse and neglect, the average amount is roughly the cost of a car payment. Today’s for-profit nursing home facility rakes in millions annually. Most of that revenue comes from taxpayers, through the Centers for Medicare & Medicaid (CMS), which also oversees inspections and fines of nursing homes. Without heavier fines and stricter enforcement, the only real deterrent for nursing home abuse and neglect in Maryland is the threat of a lawsuit from a nursing home abuse attorney.
To schedule a free case review with a nursing home negligence lawyer serving Baltimore, call Brown & Barron at (410) 698-1717 or contact us online today!
If you want more articles like this, subscribe to our free monthly newsletter by clicking here.
The Average Fine at Maryland Nursing Homes
CMS, especially Medicare, oversees the nursing home industry, and they publish detailed reports of inspections, including fines and payment suspensions. Using public CMS data, ProPublica, an advocacy organization, has provided these statistics on the violations and fines at Maryland nursing homes.
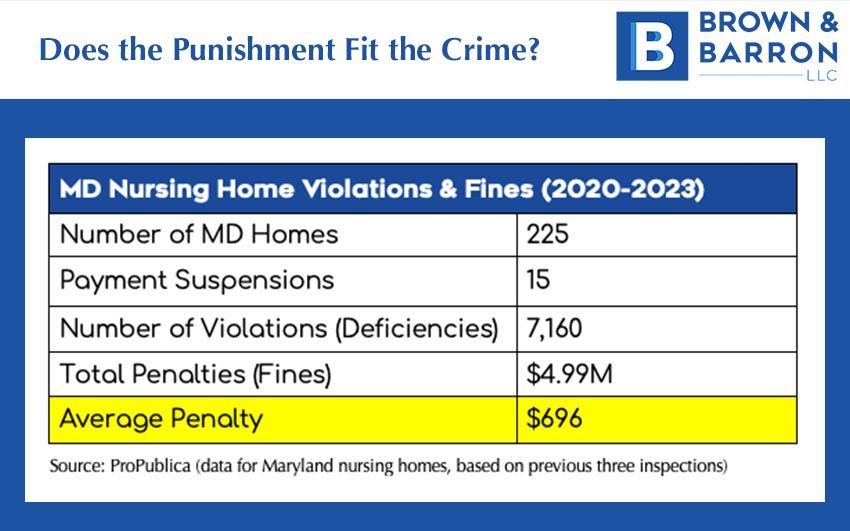
According to IBISWorld, the average nursing home facility generates nearly $4 million per year in revenue, so a measly $696, is not going to have a huge impact on their bottom line. Assuming the facility’s ownership doesn’t care about the misery and death of residents, it is more profitable to simply pay the fines than it is to invest in adequate staff, training, and procedures. And that’s exactly what happens.
Vile Forms of Abuse Get Small Fines
Nursing home violations are graded A through L. The more severe grades (and fines) are given to potentially deadly situations to one or more residents. That means that some of the most disgusting incidents of abuse and neglect typically fall into the “minor” grade of violations. Heinous violations often get the smaller fines, because they are typically isolated to individual residents and aren’t considered life-threatening. This can include things like:
- Verbal & physical abuse
- Bullying & intimidation
- Neglect (e.g., residents left for hours or days in urine and feces)
- Theft
- And more
That’s assuming these violations are documented and enforced. Many residents are too infirm to remember or too afraid to report incidents. Plus, the inspections have a bad reputation for giving nursing homes far too many warnings. Nursing homes also have a very nursing-home-friendly appeals process for serious offenses. It’s a bureaucratic process with poor transparency and follow-through, enabling the worst abuses to get swept under the rug.
In an investigative report on the nursing home inspection and appeals process, the New York Times said this:
Even when the citations are upheld by this federal court, some never make their way onto the Medicare website, known as Care Compare. In November, for example, the courtsustained a major punishment against Life Care Center of Kirkland, Wash. — the nursing home that faced the first coronavirus outbreak in the United States — yet the citation is absentfrom the Medicare site. The facility has a five-star rating.
The pattern gives nursing homes a powerful incentive to pursue every available appeal. Even if they lose, the process eats up time and reduces the odds of damaging information ever becoming public.
(Robert Gebeloff, Katie Thomas and Jessica Silver-Greenberg, in the New York Times)
Who Charges the Fines?
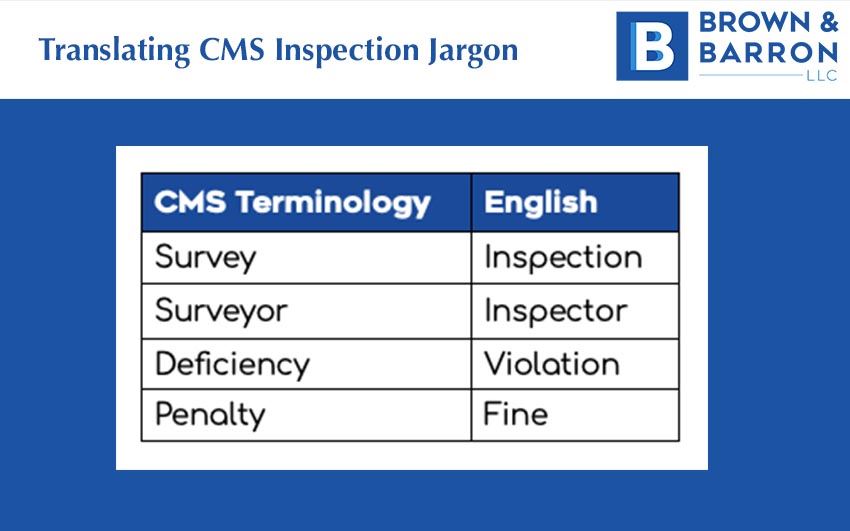
There are annual surprise inspections (CMS calls them surveys) at nursing homes that get Medicare & Medicaid taxpayer dollars. There are set federal and state regulations they must follow to ensure the safety and quality of life of residents. As low as these standards are, most nursing homes do not try hard to follow them. The inspectors (surveyors) can give them a warning or charge them a fine (penalty) for any violations (deficiencies) of the state and federal regulations.
Short-Staffing & Infection Control Issues
Over the past 20 years, private equity investors began buying up independent nursing homes to get in on the gravy train of guaranteed income from CMS and Baby Boomers requiring nursing home care in huge numbers. This consolidation of the nursing home industry to corporate, for-profit ownership has coincided with cost-cutting, a huge drop in quality, and higher rates of injury and deaths at nursing homes. The reason is greed. Cutting corners, with very little concern for paltry fines or resident safety, is the key to increasing profits. The two biggest problems are understaffing and infection controls.
Inspectors regularly cite Maryland nursing homes for understaffing. There is a minimum number of nursing home care professionals (CNAs), as well as other more highly trained medical personnel that the nursing home must on staff, depending on the number of residents. Nursing homes save payroll costs by inflating their staff numbers (i.e., lying to inspectors) or just paying the fines for understaffing.
The result is that there is too much work for too few staff members. This translates into burnout, high turnover to untrained personnel, mistakes (often deadly), neglect due to lack of available personnel, and abuse from stressed-out staff members. All of this cost-cutting and corner-cutting equates to horrible conditions for residents.
The New Yorker investigated the effect of private equity ownership of nursing homes. They found:
Cost-cutting is to be expected in any business, but nursing homes are particularly vulnerable. Staffing often represents the largest operating cost on a nursing home’s ledger. So, when firms buy a home, they cut staff. However, this business model has a fatal flaw. “Nurse availability,” Gupta and his colleagues wrote, “is the most important determinant of quality of care.”
At homes with fewer direct-care nurses, residents are bathed less. They fall more, because there are fewer hands to help them to the bathroom or into bed. They suffer more dehydration, malnutrition, and weight loss, and higher self-reported pain levels. They develop more pressure ulcers and a greater number of infections. They make more emergency-room visits, and they’re hospitalized more often. They get all kinds of problems that could be prevented,” Charlene Harrington, a professor emeritus of sociology and nursing at the University of California, San Francisco, said, of residents at homes with lower nurse-staffing levels. “It’s criminal.”
(Yasmin Rafiei, The New Yorker)
Understaffing Is a Vicious Cycle
With the best nursing home workers quitting the industry in droves because they’re underpaid and overworked, nursing home facilities are often left with a staff that is not only undermanned, but under-trained and unmotivated. Lack of motivation and training leads to poor infection controls, which are put in place prevent the spread of contagious illnesses. Most nursing homes inspected have repeated violations for infection controls.
The spread of bacterial and viral illnesses wreak havoc on nursing homes. They have an elderly population, people in close proximity, and they often have compromised immune systems. It’s no surprise that nursing home residents had the most COVID-19 deaths during the pandemic, even when compared to elderly people who live outside nursing homes. Nursing homes were Ground Zero for the pandemic because of decades of lax infection controls and cost-cutting.
How to Deter Nursing Homes from Abuse & Neglect
The for-profit approach to nursing home care combined with toothless enforcement leads to daily misery and death for elderly residents, and everyone in the industry knows it. Without effective enforcement and fines that actually hurt the nursing home’s bottom line, greedy nursing homes will continue to let residents suffer and die. Until a nursing home abuse lawyer comes knocking on the door with a nursing home negligence lawsuit, the nursing home will cut staff and services to the bone to raise profitability, while gladly paying the minuscule fines as a small cost of doing business.
To schedule a free case review with a nursing home negligence lawyer serving Baltimore, call Brown & Barron at (410) 698-1717 or contact us online today!


